Ingenious: Molecular Prosthetics
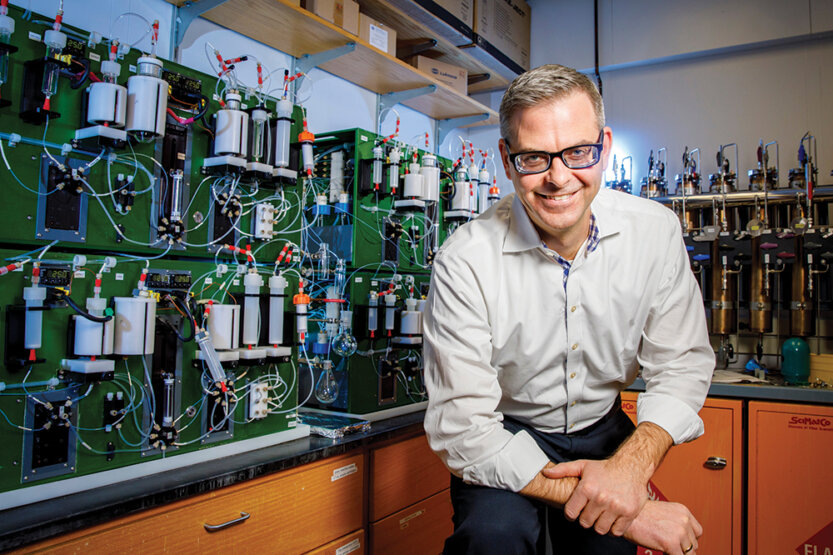 "There's so much potential with molecular prosthetics," says chemistry professor Martin Burke. (Image by Fred Zwicky_
"There's so much potential with molecular prosthetics," says chemistry professor Martin Burke. (Image by Fred Zwicky_ When Martin Burke, M.D., was making his rounds at Harvard Medical School in 1999, he visited a young woman suffering with cystic fibrosis, a genetic disease that can severely damage the lungs. As he began drawing a diagram on the whiteboard in her room explaining how a dysfunctional—or absent—protein in her body had led to her chronic condition, she stopped him and said, “‘It sounds like you know exactly what’s wrong with me. Why can’t you fix it?’” Burke recalls.
That encounter resulted in Burke becoming a chemistry professor at Illinois, where he began searching for a way to “fix it.”
As Burke explains it, almost everyone is born with the fibrosis transmembrane conductance regulator (CFTR) protein, which secretes anions (negatively charged ions) that help keep the lungs bacteria-free, among other functions. But in people with cystic fibrosis, that protein is either damaged or missing.
If individuals have the CFTR protein but it is malfunctioning, existing treatments can significantly improve their condition. But roughly 10 percent of those with cystic fibrosis don’t have the CFTR protein. There has been no treatment for them—until now.
Burke has pioneered “molecular prosthetics”—small molecules that can replace missing or damaged human proteins—with a goal to help that “untreatable” 10 percent of cystic fibrosis patients. In the same way that an artificial limb can replace a human arm or leg, the molecular prosthetic developed in Burke’s lab can replace the missing CFTR protein.
The breakthrough therapy went into Phase I clinical trials in 2023. In preparation for those trials, Burke and Michael J. Welsh, M.D., from the University of Iowa, co-founded a company called cystetic Medicines, where their chief technical officer, Jeffry Weers, Ph.D., converted the molecular drug into a powder placed inside small capsules.
The capsules are designed to be inserted into an inhaler, Burke explains. When the inhaler is pressed, the capsule punctures, turning the powder into a breathable aerosol. Aerodynamically, the aerosol particles are like nanoscale wiffle balls that float deeply into the lungs. The team began testing the inhaler with patients in November 2023.
Burke says the beauty of developing small molecules into molecular prosthetics is that they can be produced in large quantities, which drives down their cost and makes them affordable. “You can make them on the metric-ton scale,” he says. “You can put them in a bottle or pill or inhaler and send them around the world because they’re stable at room temperature. They go into your body and do something useful, and your body never knows they’re there.”
He adds, “This is just the tip of the iceberg. There are hundreds of human diseases caused by a missing protein, and in most cases, there are zero cures. But there’s so much potential with molecular prosthetics. It’s a very exciting time.”



